Where AIDS is a family affair

Patients at Siaya District Hospital
Kogelo, Kenya -- Accompanied by two HIV counselors, we left the Kogelo Dispensary, walked down a dirt road for a little while, and then veered off down a path that twists among trees and fields. Soon enough, we came to a family compound with a few large earthen huts, home to the family of John Ongiri. This isn’t an easy place for public-health programs to reach, but nearly 15 percent of people in the surrounding Nyanza Province are thought to be HIV-positive. In no small way, the effort to contain AIDS in the world depends on what happens in settings like these.
The US Centers for Disease Control and Prevention understands this. In conjunction with the Kenya Medical Research Institute, the CDC has hired counselors to visit homes in a designated survey area and test those over age 15 and children whose mothers are HIV-positive or deceased.
Two days before, counselors had come to the Ongiri compound; the only one to test positive was Catherine, 44, the third wife of family patriarch John, 78. Counselors Georgina Oyende and Florence Aluodo came back to check in on the family. To complicate matters, Catherine is mostly deaf and cannot speak intelligibly, though first wife Banta Ongiri, 63 - who initially invited the counselors to the family home - says that she manages to communicate with Catherine. (The two counselors translated for the Ongiris.)
I visited the compound as part of a trip for US editors organized by the International Reporting Project. Our visit revealed how much HIV testing efforts need to adapt - and have adapted - to landscapes and family structures far removed from those in urban and suburban America.
Frankness by necessity
Americans who want to know their HIV status are often tested in confidential or anonymous clinics run by nonprofit groups, or in medical offices where strict privacy rules apply. This approach has its roots in the early days of the AIDS crisis in the United States, when so many of those infected were gay men who were estranged from their families. And it reflects what experts call “AIDS exceptionalism’’ - the idea that the disease remains so stigmatized that medical authorities must approach it more gingerly than other ailments.
But in Nyanza Province, the condition is all too commonplace, and there is an urgent need to prevent HIV-positive people from unwittingly infecting their HIV-negative partners. In these circumstances, sending counselors to prick the fingers of people in remote compounds becomes sensible and cost-effective. Kayla Laserson, director of the CDC’s field office in Kisumu, Kenya, says the counselors who visit homes ask residents whether they prefer to be tested individually - or at all. But she says counselors encourage families to be tested together; family members can more easily disclose their status to one another, and if need be they can help each other in seeking medical care and adhering to treatment regimens.
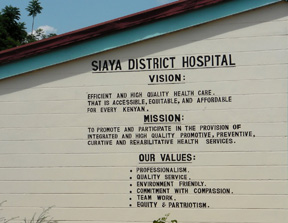
Siaya District Hospital.
The Ongiris had begun telling the oldest of Catherine’s five children about her condition. As I sat in John and Banta’s hut, it seemed odd to hear the family discuss Catherine’s status so evenhandedly, especially since the news was so fresh. When one member of a couple tests positive and the other does not, counselors stress that this discordance is not a sure sign of infidelity. John and Banta understood this. Still, they wondered what could have happened; their thoughts turned to unclean cuts, shared razor blades, and the possibility that Catherine was HIV-positive when she became the third wife in 1993.
The possibility of domestic discord lurks in counselors’ observations about other homes they have visited. Some women have already sought testing surreptitiously. Some men, they say, will assent to having their wives and children tested but will refuse themselves. The counselors I accompanied were businesslike and supportive in equal measures; counselor Georgina Oyende, HIV-negative at 32, became interested in the CDC work after losing her husband to the virus. Counselors clearly need such empathy, and they need to think on their feet.
An anti-retroviral revolution
Demand for testing is high in communities across sub-Saharan Africa, now that drugs to treat HIV are more widely available. Donald Thea, a Boston University School of Public Health professor who isn’t involved in the CDC effort but has worked with HIV-testing programs in Zambia, says that in the last five years “the game changed completely.’’ The cost of anti-retroviral treatment has plunged from $17,000 a year to no more than $200.
The spread of these drugs, he says, increases the “ethical justification for pushing services out into the community.’’ Thea also says some healthcare workers in Zambia began to worry about promoting a stigma around HIV by approaching it differently from other infectious diseases.
The home visits that the CDC sponsors in Kenya don’t preclude other ways of dealing with what remains an epidemic. Not far from Kogelo, for instance, employees at the Siaya District Hospital have discreetly reached out to the few men who acknowledge having had sex with other men and asked them to refer friends for testing and treatment. This approach strongly recalls early anti-HIV efforts in the United States.
The CDC’s family-based approach, in contrast, represents a studied response to a much different type of epidemic. In this part of Kenya, American-style medical individualism goes only so far.
More from this Reporter
From Other Reporters in This Country
Also appeared in…
- The Boston Globe
